Signs and Symptoms of Amniorrhexis in Expectant Mothers
Pregnancy is a time of profound change for a woman’s body, but it’s also a delicate period that requires attention to even the smallest shifts. Among the many potential concerns is the rupture of the fetal membrane, a condition known as amniorrhexis. This often under-discussed condition is the leading cause of preterm labor, making it crucial for expectant mothers and healthcare professionals to be well-versed in its signs and implications. We’ll explore the signs and symptoms of amniorrhexis in expectant mothers to arm you with the knowledge you need to recognize it and explain why early detection is vital for mother and child.
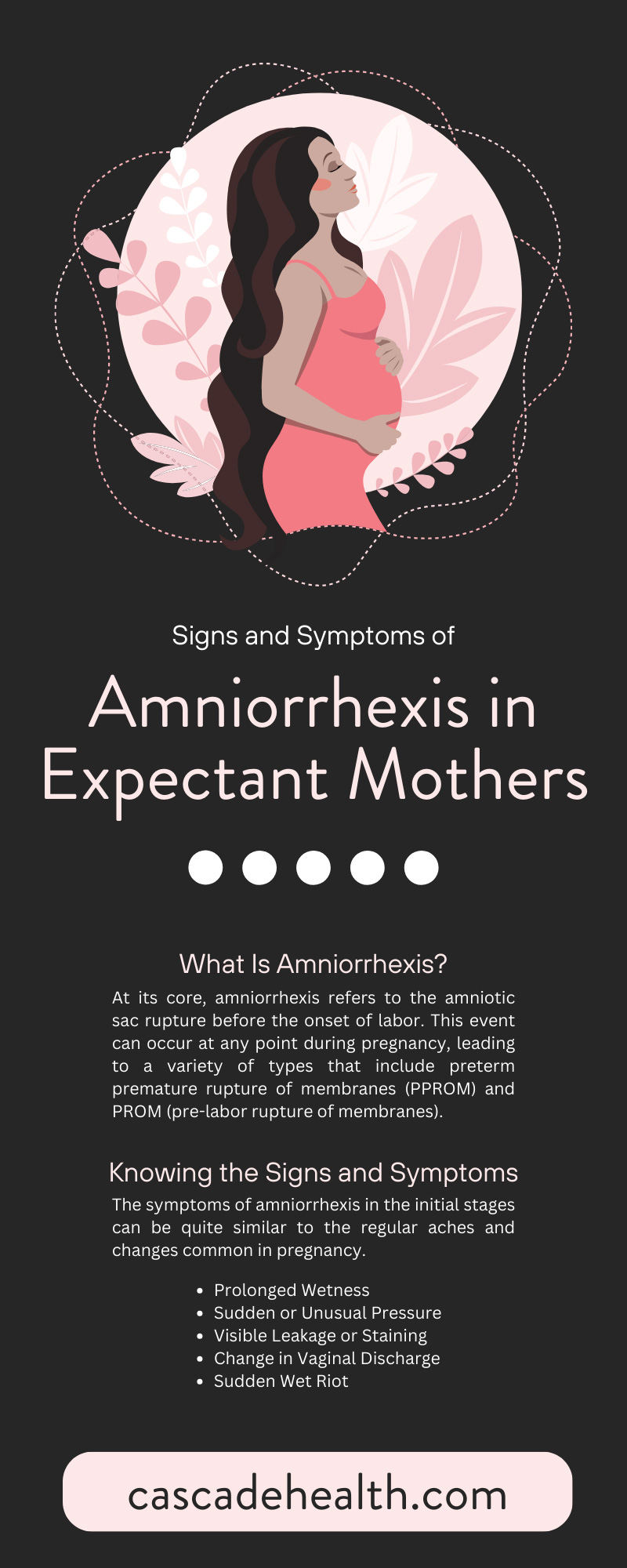
What Is Amniorrhexis?
At its core, amniorrhexis refers to the amniotic sac rupture before the onset of labor. This event can occur at any point during pregnancy, leading to a variety of types that include preterm premature rupture of membranes (PPROM) and PROM (pre-labor rupture of membranes). Despite the gravity of the situation, distinguishing it from regular pregnancy symptoms can be challenging. Understanding it requires a closer look.
The amniotic sac plays a vital role in pregnancy, protecting the fetus and acting as a cushion against injury. Its rupture can release amniotic fluid, which often presents as a gush or a trickle—the familiar “water breaking” that many movies and popular culture often associate with labor. But the signs can be more subtle and easily overlooked.
Knowing the Signs and Symptoms
The symptoms of amniorrhexis in the initial stages can be quite similar to the regular aches and changes common in pregnancy. However, key indicators exist that should raise flags for expecting mothers.
Prolonged Wetness
Sudden wetness that continues or recurrent instances of dampness unrelated to urinary incontinence can be an early sign of amniorrhexis. This wetness may not always be dramatic, but continuous dampness or the frequent need to change pads due to moisture is a red flag.
Sudden or Unusual Pressure
A sensation of pressure in the pelvic region, especially when accompanied by dampness, can signify amniotic fluid leaking. Many often describe this pressure as heaviness or fullness.
Visible Leakage or Staining
Visible fluid leakage from the vagina that is clear, pale yellow, or tinged with blood bears all the hallmarks of amniotic fluid, signaling a potential rupture. Staining on undergarments, even in small amounts, should prompt a visit to the healthcare provider.
Change in Vaginal Discharge
Pregnancy often leads to increased vaginal discharge, but you should heed a sudden and significant change. Discharge that transforms into a watery consistency could indicate amniorrhexis.
Sudden Wet Riot
Perhaps the most cinematic of the telltale signs, a dramatic gush of fluid from the vagina is a clear indicator of amniotic fluid release. Labor contractions immediately follow in some cases; in others, the rupture may not lead to immediate labor.
Diagnostic Methods and When To Seek Medical Attention
Rapid and accurate diagnosis is a linchpin for healthcare professionals managing amniorrhexis. They typically use clinical assessment and diagnostic testing to confirm the diagnosis.
Clinical Examination
A comprehensive history is the first line of defense, followed by a physical examination where specific techniques can test for the presence of amniotic fluid. A nitrazine test is one of the most common tests, which uses litmus paper to determine the pH level of vaginal secretions; amniotic fluid is alkaline. Ferning patterns that appear under a microscope can also indicate amniotic fluid in a sample.
Ultrasounds
Ultrasounds can directly view the amniotic sac and confirm a rupture, especially when the ultrasound technician assesses the liquid index. An ultrasound can also help gauge the baby’s gestational age, an essential tool when managing PPROM and related complications.
Amniocentesis
Amniocentesis is an invasive but highly accurate test where a medical practitioner inserts a needle to collect amniotic fluid. Many neonatal care professionals consider this test when other diagnostic methods yield indeterminate results or when they must confirm the fetus’s gestational age.
Early detection and prompt medical attention are critical for managing amniorrhexis. Encourage expecting mothers to not delay the decision to seek medical help to ensure the best outcomes for themselves and their children.
Impact of Amniorrhexis on Pregnancy and Delivery
The implications of amniorrhexis are wide-reaching, with potential effects on the remainder of the pregnancy, labor, and the child’s long-term health.
Preterm Labor
Amniorrhexis events that occur before the 37th week of pregnancy can lead to preterm labor, a significant risk factor for complications that include respiratory distress, infections, and long-term health issues in the child. The situation is particularly critical in cases of PPROM, and immediate hospitalization is often necessary.
Infection Risk
The amniotic sac acts as a barrier to infection. Its rupture can allow bacteria to enter the uterus and, consequently, the amniotic fluid, posing a serious risk to the health of the mother and fetus. Monitoring for signs of infection, such as fever or increased heart rate, is paramount.
Need for Induction
Amniorrhexis can trigger labor, but medical intervention may be necessary to reduce the risk of infection in cases where it does not. Induction is necessary to prevent complications that can arise from prolonged amniotic fluid leakage.
Support and Care for Expectant Mothers
With the weight of potential complications looming, support and preparedness become critical aspects of care for expectant mothers facing amniorrhexis.
Emotional Support
The diagnosis of amniorrhexis can be frightening, but midwives and other neonatal professionals should reassure expecting mothers that they’re not alone. Emotional support from partners, family members, and their healthcare team is essential in navigating the complex emotions and uncertainties that arise.
Physical Preparedness
Understanding the next steps is crucial. Midwives and other neonatal professionals should inform expectant mothers of the possibility of induction, the process of labor, and potential NICU stays for their children. Knowledge empowers mothers to participate actively in their care and that of their newborns.
Lifestyle Adjustment
You may prescribe bed rest or restricted activity to prevent preterm labor. Making these adjustments, however challenging, can significantly improve the chances of a healthy full-term delivery.
The signs and symptoms of amniorrhexis in expectant mothers are subtle but significant, demanding the attention of the mother and their professional healthcare team. Early detection and intervention are the bedrock for ensuring the health and safety of mother and child. Check out Cascade Health Care’s selection of medical instruments, including our amniotic hooks, today. We can mitigate amniorrhexis effects and work toward achieving successful, full-term deliveries by fostering awareness, providing information, and encouraging a proactive approach to pregnancy.
Recent Posts
-
The History and Evolution of the Speculum
Most women view the speculum as a symbol of modern routine healthcare, a cold but necessary instrume
-
What Midwives Should Teach New Parents Regarding Breastmilk
The transition into parenthood presents a profound physiological and emotional shift for growing fam



