Safety Considerations When Using Amnicots for Amniotomy
Amniotomy, a procedure used in obstetrics to artificially rupture the amniotic sac, requires precision, expertise, and strict adherence to safety protocols. This practice often induces or accelerates labor when labor progression is stalled or other medical indications arise.
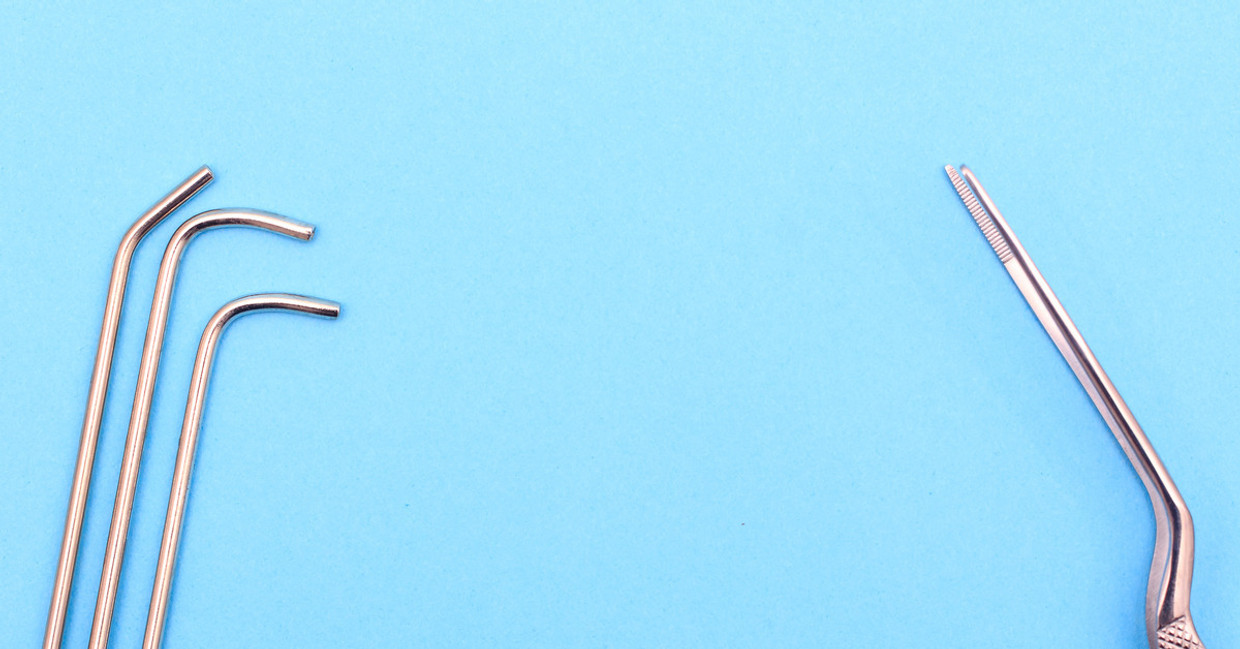
One of the key tools for performing an amniotomy is the amnicot—a small, finger-mounted device designed to assist obstetricians and midwives during the procedure. While the tool is simple in design, its correct handling and application are crucial to ensuring the safety of the patient and the fetus. We’ll discuss safety considerations when using amnicots for amniotomy.
Ensure Sterile Technique
Maintaining a sterile environment is non-negotiable when performing amniotomy. The amnicot must be handled using sterile techniques to prevent the introduction of potentially harmful bacteria into the amniotic sac or uterus.
Before the procedure, all necessary equipment, including the amnicot, should be sterilized or come in single-use sterile packaging. Practitioners must thoroughly wash their hands, wear sterile gloves, and follow established protocols to guard against infection. This protects the patient and ensures the safety of the healthcare provider performing the procedure.
Proper Placement of the Amnicot
Correct placement of the amnicot on the practitioner’s finger is paramount. Improper positioning could increase the likelihood of accidental trauma to the membranes or surrounding tissues.
Before initiating the procedure, the practitioner should carefully fit the amnicot over their finger and ensure the tool sits comfortably and securely. During use, avoid applying excessive pressure, and proceed with gentle, controlled movements to minimize risks to the amniotic sac and the patient’s cervical and vaginal tissues.
Patient Monitoring
Consistent monitoring is key during any obstetric procedure; amniotomy is no exception. Patients should be monitored continuously to track vital signs and fetal heart rate before and during the procedure. After the amniotomy has been performed, additional monitoring is equally critical to detect any signs of distress or complications, such as excessive bleeding or infection.
Fetal monitoring is critical, ensuring that the baby tolerates the procedure well. Observing for any decelerations or irregularities in the fetal heart rate provides real-time insight into fetal well-being, enabling immediate action if required.
Assessment of Indications
Before proceeding with an amniotomy, the practitioner must carefully assess the medical indications and ensure the procedure is warranted. Clinicians should consider factors such as stalled labor progression, fetal positioning, or the presence of medical conditions that necessitate amniotomy to ensure that it is the best course of action.
Equally as important is patient consent. Practitioners must explain the procedure, risks, and benefits to the patient to allow them to make an informed decision. Clear communication creates trust between the patient and practitioner, forming the foundation of excellent care.
Adhering to Best Practices
Safety should always be the guiding principle in obstetrics, and this rings especially true for amniotomy procedures using amnicots. By following proper safety precautions when using amnicots, medical professionals can uphold the highest safety standards.
Continuous education and professional development are essential for refining and improving clinical skills. If you’re looking for reliable amniotomy tools, explore Cascade Health Care's selection of amnicatorsdesigned with practitioners in mind.
Recent Posts
-
Best Practices for Cleaning and Maintaining Pulse Oximeters
Midwives and medical professionals understand the critical nature of accurate patient data. When mon
-
What To Do With Birthing Supplies After a Home Birth
Home birth is on the rise. As families increasingly seek the comfort and autonomy of birthing in the