Recognizing and Troubleshooting Common Pulse Oximeter Errors
Pulse oximetry is an indispensable tool in modern healthcare. Used across medical settings, it provides a quick, non-invasive way to measure oxygen saturation (SpO2) and monitor a patient’s respiratory health. Critical care and outpatient clinics rely on pulse oximeters daily to guide vital clinical decisions.
Despite their ubiquitous use, improper handling and external factors can lead to inaccurate readings, compromising patient care. Healthcare professionals need to ensure every reading contributes accurately to diagnosis and treatment. This guide explores the fundamentals of pulse oximetry, the significance of proper usage, and practical steps for recognizing and troubleshooting common pulse oximeter errors.
What is Pulse Oximetry, and Why Is It Important?
Pulse oximetry is a method of measuring the oxygen saturation in a patient’s blood. By shining infrared light through the skin and analyzing the amount absorbed, pulse oximeters offer insights into the oxygenation status of hemoglobin. This instrument is non-invasive, portable, and ideal for continuously monitoring oxygen levels without requiring invasive procedures, such as arterial blood sampling.
Healthcare providers utilize pulse oximeters across a variety of clinical scenarios. From assessing oxygen levels in patients during surgical anesthesia to monitoring chronic conditions such as COPD, the device is a critical bridge between timely diagnosis and intervention.
Understanding How Pulse Oximeters Work
Understanding how pulse oximeters function is key to optimizing their usage. These devices rely on photoplethysmography, which involves shining light through the skin and analyzing changes in light absorption caused by blood flow. By distinguishing between oxygenated and deoxygenated hemoglobin based on light intensity, the device provides an SpO2 percentage.
Typically, the device fits securely onto a fingertip, toe, or earlobe—areas where blood flow is easily detectable. A pulse oximeter works best when skin is clean, free from barriers, and adequately perfused for accurate readings.
Why Proper Use Is Essential
For reliable measurements, healthcare professionals must know how to use and troubleshoot pulse oximeters effectively. Errors in usage can lead to misdiagnoses, unnecessary interventions, or overlooked conditions, directly impacting patient safety.
The complexity of healthcare environments, changing lighting conditions to patients' physiological states, further emphasizes the need to understand and address potential pitfalls when using oximeters. A proactive approach ensures accurate readings and builds confidence between professionals and their diagnostic tools.
Troubleshooting Common Pulse Oximeter Errors
Identifying and addressing common pulse oximeter errors is crucial in maintaining accuracy and effectiveness. Below are practical tips to troubleshoot issues and ensure precise readings every time.
Ensure Proper Device Placement
Proper placement is the foundation of accurate pulse oximetry, ensuring reliable and consistent readings. If the probe is misaligned or too loose, it can result in inaccurate measurements that may mislead healthcare providers. Such faulty readings can pose significant risks to patient care, emphasizing the importance of correct probe positioning.
- Best Practice: Secure the device snugly, aligning it with the fingertip’s pad. Avoid uneven placements that could obstruct light pathways.
Check for External Light Interference
Bright ambient light can interfere with the device’s sensors, causing disruptions in their functionality. This interference can lead to fluctuating or inaccurate readings, which may affect the reliability of the data. To ensure accurate performance, minimize exposure to excessive light during use.
- Best Practice: Conduct measurements in areas with controlled lighting. If natural light is unavoidable, cup your hand gently over the device to block excess light.
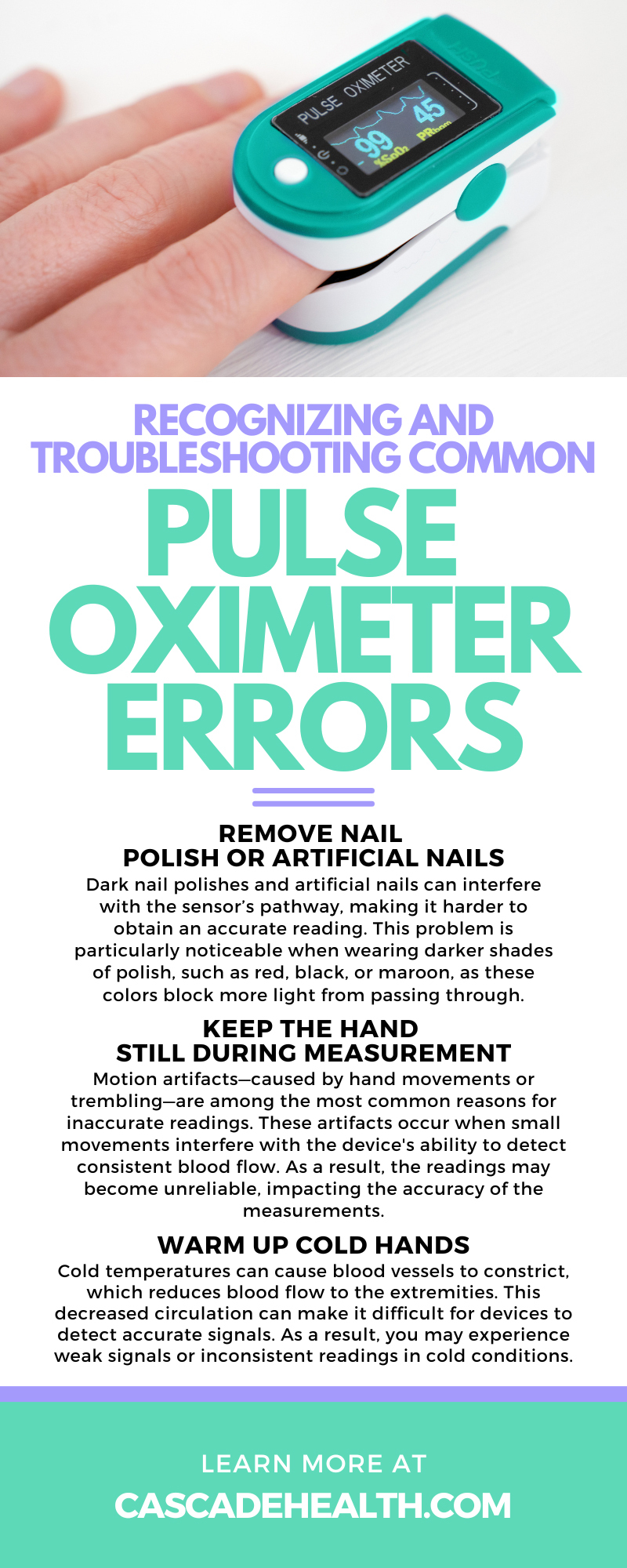
Remove Nail Polish or Artificial Nails
Dark nail polishes and artificial nails can interfere with the sensor’s pathway, making it harder to obtain an accurate reading. This problem is particularly noticeable when wearing darker shades of polish, such as red, black, or maroon, as these colors block more light from passing through.
- Best Practice: Request patients remove polish or artificial nails before measuring. Use an alternate site such as the side of the finger or an earlobe.
Keep the Hand Still During Measurement
Motion artifacts—caused by hand movements or trembling—are among the most common reasons for inaccurate readings. These artifacts occur when small movements interfere with the device's ability to detect consistent blood flow. As a result, the readings may become unreliable, impacting the accuracy of the measurements.
- Best Practice: Ensure patients remain still during measurements. Encourage relaxation and use additional support to stabilize the hand if needed.
Warm Up Cold Hands
Cold temperatures can cause blood vessels to constrict, which reduces blood flow to the extremities. This decreased circulation can make it difficult for devices to detect accurate signals. As a result, you may experience weak signals or inconsistent readings in cold conditions.
- Best Practice: Ask the patient to warm their hands before taking a reading. Simple methods include rubbing their hands together or briefly running warm water over them.
Avoid Excessive Pressure on the Sensor
While securing the device properly is important, you should avoid overtightening. Tightening the device too much can compress blood vessels, which may restrict blood flow. This can lead to discomfort or even inaccurate results, compromising the effectiveness of the measurement.
- Best Practice: Adjust the clamp to ensure the probe is snug but not overly tight. A device that feels comfortable but secure will likely give the most accurate results.
Monitor Battery and Device Condition
Low battery levels can lead to inconsistent or erratic device performance, causing interruptions when you need your device most. Over time, physical wear and tear can further impact the functionality and reliability of your device. Together, these issues can significantly reduce your technology's overall efficiency and lifespan.
- Best Practice: Regularly inspect the device for signs of damage. Keep spare batteries available and test the device frequently for optimal reliability.
Be Aware of Motion Artifacts
Motion, including trembling or active movements, disrupts the device’s ability to capture steady signals. This interference occurs because the device relies on stability to detect and process data accurately. Without stillness, the signals become inconsistent and unreliable, impacting overall performance.
- Best Practice: Position patients comfortably and remind them to avoid movement during measurements.
Verify Against Clinical Symptoms
Pulse oximeters are valuable tools, but they should never replace clinical judgment. While they provide important data, relying solely on these devices can lead to the oversight of broader health issues. Using them in conjunction with a comprehensive clinical assessment for accurate decision-making is essential.
- Best Practice: Always interpret readings alongside the patient’s symptoms and visual indicators to capture the full clinical picture. Look for signs of labored breathing or changes in skin color.
Prioritize Accuracy and Confidence in Pulse Oximetry
By learning how to troubleshoot common pulse oximeter errors, healthcare professionals can confidently leverage this tool’s potential. Reliable readings ensure timely interventions, fewer missteps, and enhanced patient care.
For the best results in your practice, consider upgrading your devices with trusted options. Check out the pulse oximeters offered by Cascade Health Care, designed for precision and reliability in every clinical setting.
Recent Posts
-
Tips for Maintaining Milk Supply When Returning to Work
Returning to work after welcoming a baby introduces logistical, emotional, and physiological challen
-
9 Items EMTs Should Have Stocked for Prehospital Deliveries
Prehospital deliveries rarely announce themselves with perfect timing. One minute you take a routine



